Supporting the Move to Minimally Invasive Surgery
In 2019, 57.2% of hysterectomies in the UK were performed as open (abdominal) procedures, despite significant disadvantages at both a hospital and patient level when compared with minimally invasive alternative approaches.
In 2019, 57.2% of hysterectomies in the UK were performed as open (abdominal) procedures, despite significant disadvantages at both a hospital and patient level when compared with minimally invasive alternative approaches.
Minimally invasive surgery, also known as laparoscopic, is proven to have significant patient benefits. Patients who have a laparoscopic hysterectomy generally have a significantly reduced length of stay when compared to open procedures of up to 4 days. Recovery is also enhanced; patients can return to work and resume normal routines faster than the standard abdominal hysterectomy recovery time of 6 to 8 weeks. (1)
As well as these significant patient benefits, there are clear financial benefits of laparoscopic surgery over open surgery. Reduction in length of stay can save up to £431 per day. Admissions to Intensive Therapy Units and additional physiotherapy appointments are also reduced due to the less invasive nature of the procedure and enhanced recovery.
Despite clear advantages, many provider trusts have a lower laparoscopic surgery rate due to a number of barriers to the uptake of minimally invasive surgery.
Immediate financial pressures within the healthcare environment lead to a focus on short term targets as opposed to an “invest to save” mind set. Although the initial investment in laparoscopic instruments and visualisation systems may seem high, the savings associated with high quality and cost-effective care far outweigh this. (2)
Surgeon training and preferences also play a large part in the avoidance of laparoscopic surgery. The technical nature of performing laparoscopic surgery is such that advanced training opportunities are required. Low patient volume and lack of training leads to slower progression along the learning curve in becoming proficient at complex skills such as laparoscopic suturing. Unfortunately, access to training centres and patient volume differs geographically, leading to regional variances in skill level. (2)
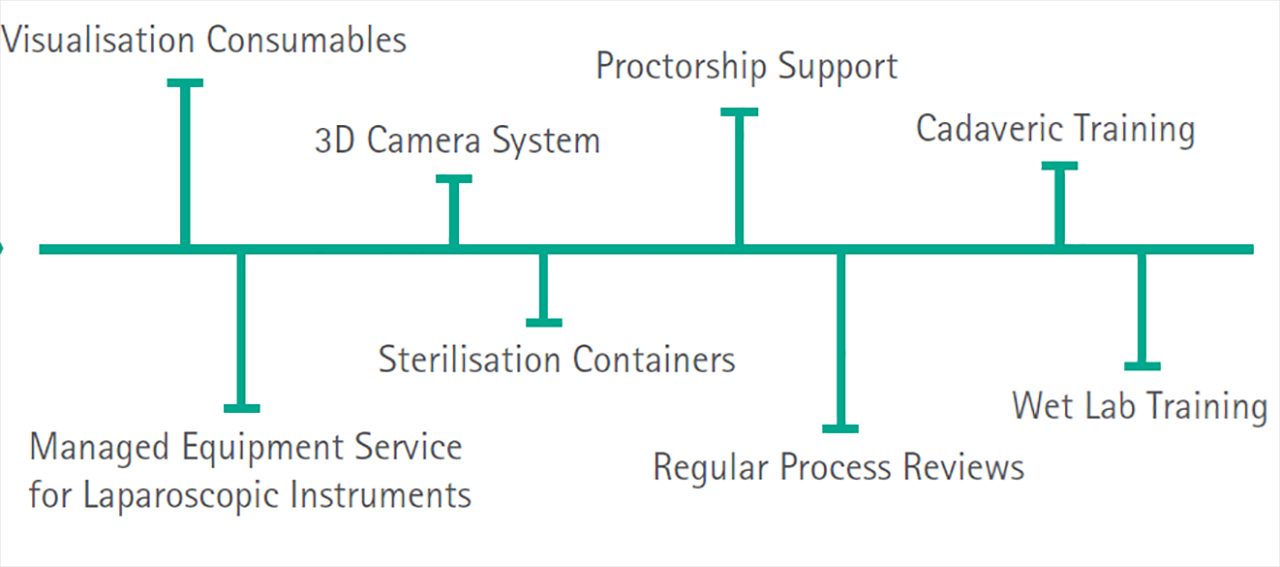
The B. Braun Laparoscopic Gynaecology pathway helps to overcome these barriers and aid the smooth transition to performing laparoscopic hysterectomies. Through access to the latest equipment and technology, specialist training courses and access to cadaveric and wet lab courses, surgeons are supported along the learning curve. In addition, the pathway includes bespoke proctorship support from the Wirral University Teaching Hospital NHS Foundation Trust, one of the top trusts in the UK with 82% of hysterectomies being carried out laparoscopically (2019-2020 Financial Year).
If you are interested in finding out more about the Laparoscopic Gynaecology partnership, please contact the Strategic Partnerships team at strategicpartnerships.bbmuk@bbraun.com.
1. NHS (2020), Having a laparoscopic hysterectomy. Online: http://bit.ly/2TPZA19 [Accessed 9th March 2020]
2. Cole, A., O’Neill, P., Sampson, C., and Lorgelly, P. (2018) Barriers to Uptake of Minimal Access Surgery in the United Kingdom, Office of Health Economics. Online: http://bit.ly/2PXED32 [Accessed 9th March 2020]