Benefits of Debridement Pads in Clinical Practice
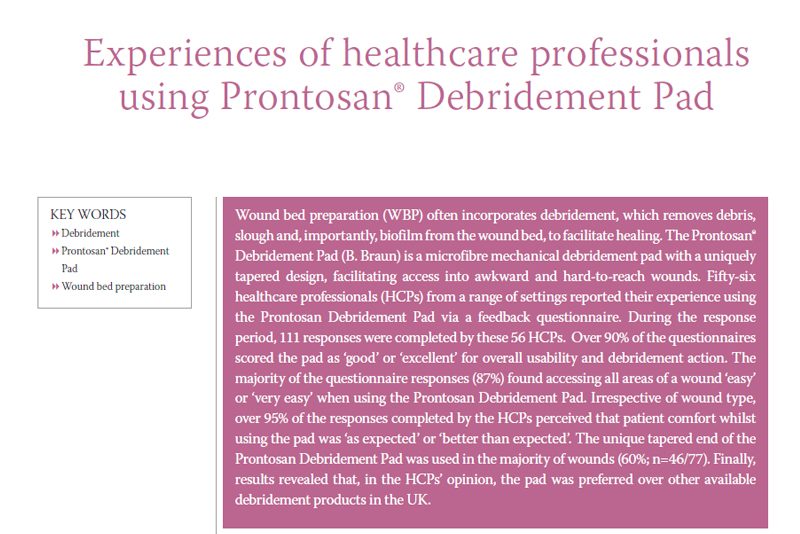
During the inflammatory phase of healing slough and exudate is produced, in chronic wounds excess exudate and the presence of slough can impede healing and contribute to biofilm production. Wound Bed Preparation (WBP) aims in the reduction of debris and bioburden from a wound bed via the removal of devitalised tissue, slough and exudate.
Wound cleansing and debridement are separate treatment stages: cleansing of the wound bed aims to loosen devitalised tissue, debris and biofilm, which is often performed as a soak or irrigation, with the use of surfactant-containing cleansers encouraged. Debridement usually follows cleansing, facilitating the removal of non-viable tissue, biofilm, slough and exudate. More than one method of debridement may be required and debridement may be repeated over a number of weeks; it has been reported that a pre-soak prior to mechanical debridement enhances the effectiveness of debridement and this combination approach works in line with wound bed preparation stages.
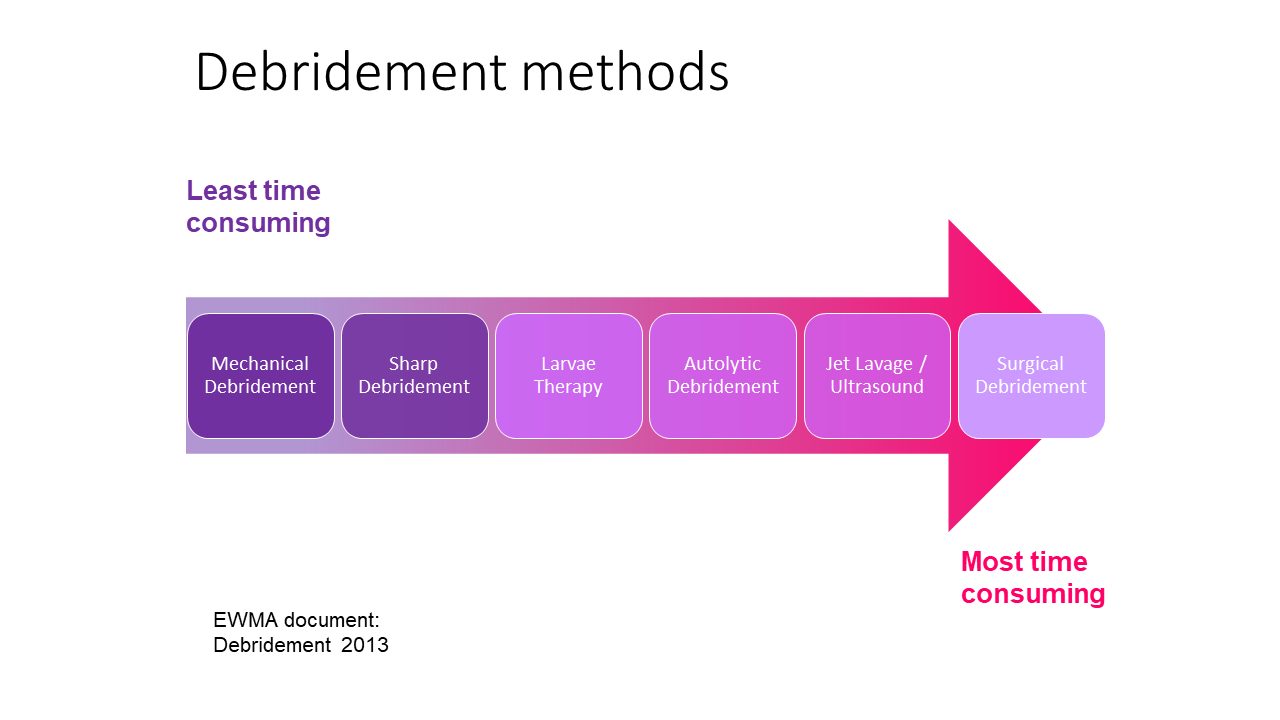
Debridement methods range from enzymatic and autolytic processes through to physical processes via mechanical or surgical debridement. However, it is only mechanical debridement that allows for physical debridement of chronic wounds without the need for specialist knowledge. Mechanical debridement has the benefit of removing non-viable tissue quickly, hence it is often an attractive option for both the patient and the healthcare professional (HCP).
It is important that any debridement product is not only effective but also easy to use by clinicians.
Patient comfort is important to achieve good patient outcomes and wound healing, since any delay in debridement can lead to increased risk of infection and other complications of non-healing. Staff may have shied away from the process of debridement leaving it to the specialist team only, with the availability of mechanical debridement pads which can be used safely in the community and across all clinical settings, so that clinicians can confidently remove the devitalised tissue from the wound bed, leaving healthy tissue intact, without causing pain and trauma to the patient, confidence in debridement is benefitting patients and the wider community setting.
Case Study
Wound bed preparation incorporating Prontosan Debridement Pad
(Kramer et al, 2018; case study courtesy of Luxmi Dhoonmoon)
This lower limb ulcer had been present for 3 years and had been static for months. Due to the patient’s pain levels, debridement was not always possible or successful. Exudate levels were causing frequent strikethrough and odour was a significant problem. Dressing changes were 2-3 times per week. Prontosan Solution was used in conjunction with the Prontosan Debridement Pad. The wound had two treatments with Prontosan Debridement Pad with significant improvement in the wound bed noted due to decreased devitalised tissue and slough. Dressing changes were reduced to once per week. The patient’s pain and odour issues improved, and the patient was more comfortable wearing their compression garments. The patient’s mobility also benefited and they were able to increase their level of exercise, which had a positive effect on their overall health. Debridement and effective wound bed preparation, which kickstarted wound healing, had a positive effect on the patient’s general health and quality of life.
This blog is an adaption of work submitted for an article original published by Wounds UK
Reference
1. Strohal, R., Apelqvist, J., Dissemond, J. et al. EWMA Document: Debridement. J Wound Care. 2013; 22 (Suppl. 1): S1–S52.