Basics of lipos
What are lipos?
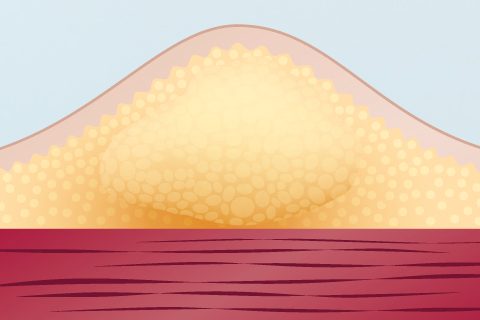
The term lipohypertrophy describes a small area where the tissue has thickened: Hard lumps of extra fat form under the skin and sometimes even scar tissue develops. However, sometimes they are invisible and only detectable by feeling your injection sites. Lipos feel bumpy or scarlike to the touch.(3)
Why do lipos occur?
Lipos are a body reaction which will occur if you repeatedly inject into the same area over a period of time. But sometimes insulin itself plays a role as well. If you inject into the same spot over and over again, residues of insulin remain in the fatty tissue and cause the fat cells to grow.(19)
The body reacts this way if you
- Repeatedly inject into the same spot.
- Reuse needles, since the tip becomes blunt and causes more of an injury.(5,6)
Why are lipos risky?
You might have heard that some people with diabetes prefer to inject into lipos. Allegedly, because you do not feel the needle entering the skin.(17) However, this is extremely dangerous. Apart from making the lipos worse and more unaesthetic, there is a higher rate of unexplained hypoglycemia and glycemic variability. Because even if you have done everything right, the insulin will not be absorbed properly.(5,6)
Recent studies have shown that if insulin is administered into lipos, it only shows 30 percent of its efficacy.(18) This phenomenon results in a need for higher insulin dosages of 10 to 15 insulin units more.(5) Make sure you talk this over with your diabetes team.
Handling lipos
How do I detect lipos?
When you meet your diabetes team, they will probably look for anomalies at the injections sites. But it is important to check your skin yourself regularly. Use two methods of examination:
1. Check your skin visually. It is also a good idea to look for
- needle insertion marks
- bruising of the skin.
2. Check your skin with your hands. If you palpate your injections sites, please ensure that you
- do this in a warm room (goose bumps make it harder to feel lipos)
- just lightly touch your skin with minimal pressure
- feel for irregularities on the skin surface and for hardened lumps which will cause your finger to rise up a little when you drag it over the area.
If you have questions or need someone to show you how to detect lipos, please do not hesitate to ask your diabetes team.
What do I do if I have lipos?
If you or your diabetes team have detected lipos, the best you can do is to stay away from that area. You should avoid injecting into any lipo or its direct vicinity for at least three months. During this period, they can reduce in size or even disappear.
Tips
Tips: knowing lipos
✔ Check yourself regularly for lipos.
✔ Do not inject repeatedly into the same spot, otherwise lipos will form.
✔ Use a needle only once, because repeated use causes lipos, too.
✔ Never inject into lipos.
✔ If you detect any anomalies, please contact your physician.
Related topics
Sources
3. Frid A. et al., New Insulin Delivery Recommendations, Mayo Clinic Proceedings, September 2016; 90(9):1231-1255.
5. Frid A. et al., Worldwide Injection Technique Questionnaire Study: Injecting Complications and the Role of the Professional, Mayo Clinic Proceedings, September 2016;91(9):1224-1230.
6. Blanco M. et al., Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetes, Diabetes and Metabolism 2013 Oct;39(5):445-53.
17. Heinemann L., Insulin Absorption from Lipodystrophic Areas: A (Neglected) Source of Trouble for Insulin Therapy?, Journal of Diabetes Science and Technology May 2010; 4(3): 750–753.
18. Famulla S. et al., Insulin Injection Into Lipohypertrophic Tissue: Blunted and More Variable Insulin Absorption and Action and Impaired Postprandial Glucose Control, Diabetes Care 2016;39:1486–1492.
19. https://www.medtronicdiabetes.com/loop-blog/lumps-and-bumps-from-insulin-therapy/, accessed on 17.08.2018, 16:56 CET.
Find a list of all sources of the website area Insulin Injection here.