Aligning treatment to the wound infection continuum – a podiatry perspective
Kim Wilde, Advanced Podiatrist at the Manchester Local Care Organisation, provides her insight into wound infection when considering the treatment of lower limb and foot wounds.
1. How do wound infections impact patients and your service?
Foot problems in people with diabetes have a significant financial impact on the NHS through primary care, community care, outpatient costs, increased bed occupancy and prolonged stays in hospital. Diabetic wounds are particularly challenging because diabetes disturbs the wound healing process by prolonging the inflammatory phase and delaying the formation of granulation tissue. Once tissue damage has occurred in the lower limb one of the main threats is infection which can be superficial or involving deeper structures such as bone. Guest 2020 highlights that 78% of diabetic foot wounds had a recorded infection1. Unhealed ulcers and foot infection are the leading cause of foot amputation with diabetic foot ulcers representing 80% of amputations.
“An amputation is devastating for a patient it can impact on them both emotionally and financially”
A minor amputation can still mean that a patient loses a large proportion of their foot which affects their mobility and reduces their independence. Sepsis is something that I have encountered a number of times in my foot ulcer patients. Sepsis can lead to tissue damage, organ failure and death. Diabetic foot infections account for approximately 20% of the sepsis cases in the United Kingdom.
2. Do you think that there is adequate awareness of wound infection among patients and health care professionals?
The quality of foot care for people living with Diabetes varies significantly around the United Kingdom. Proactive care and rapid referral to specialist services helps to prevent foot amputation. Although patient education courses are available there are limited places so not all patients have the ability to access them. Limited clinician time at the patient annual review may impact how much education patients receive about looking after their health and what to do if they develop a wound.
“When health care professionals are assessing wounds the classic signs of infection may be less obvious or absent in some diabetic foot infections.”
Pain and tenderness may be reduced or absent in patients who have neuropathy, whereas erythema may be absent in those with vascular disease. This may result in infection diagnosis being delayed. Patients who have peripheral neuropathy often do not realise they have an injury or wound due to the loss of pain sensation, they often present when they have noticed a smell or exudate coming from their foot.
3. How do clinicians know what product to use if there are signs of infection?
All diabetic foot wounds are likely to be colonised with bacteria. To diagnose a diabetic foot infection there has to be at least two of the following signs - local swelling, erythema, local tenderness or pain, local warmth and purulent discharge. There are differing severities of infection - Mild - local infection with 0.5 to less than 2 cm erythema, Moderate - local infection with more than 2 cm erythema or involving deeper structures (such as abscess, osteomyelitis, septic arthritis or fasciitis) and severe - local infection with signs of a systemic inflammatory response.
“Antimicrobial dressings such as Askina Calgitrol are initiated when the wound is at the local infection stage.”
What I like about Askina Calgitrol is that it has a higher silver content than most other silver dressings and the concentration of silver ions in the wound is maintained for 7 days at the level of 60ppm. The product consistency means it can easily be used in cavities.
Clinically infected wounds are reviewed on a weekly basis and silver usage normally occurs for 2 weeks then is stepped down. After Calgitrol has resolved the infection treatment can be ‘stepped down’ to Prontosan Gel X to maintain the improved wound condition and prevent biofilm reformation and help prevent infection. Prontosan Solution can be used throughout treatment as standard care for wound bed preparation.
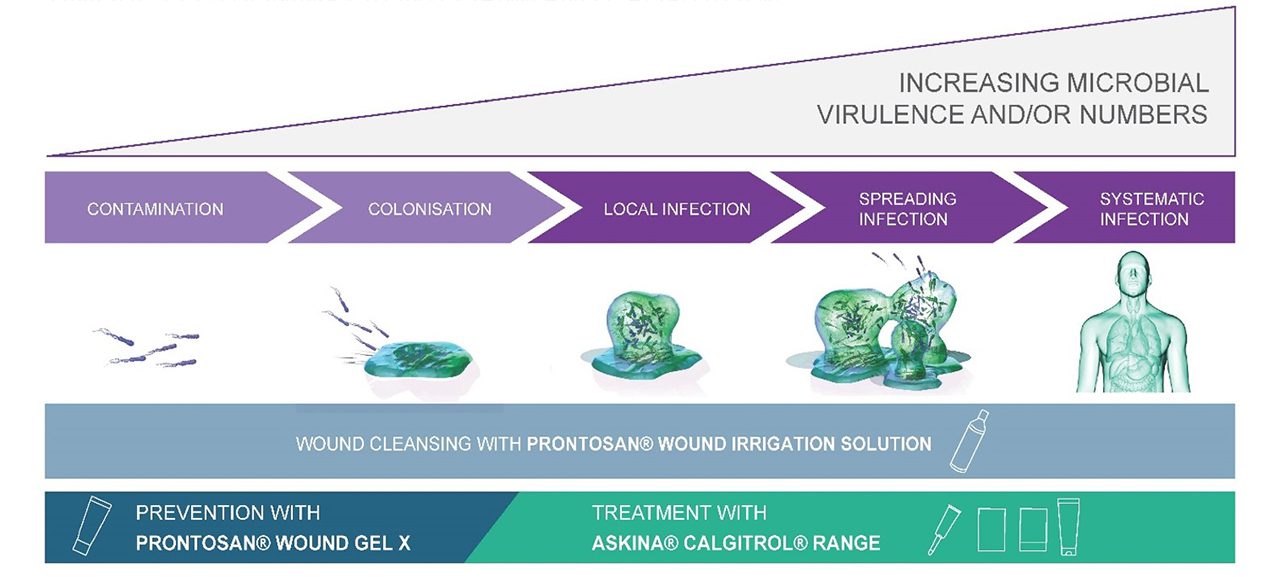
Stages of wound infection continuum – antimicrobial dressings are indicated from local infection, wound cleansing solutions can be used throughout
(Adapted from International Wound Infection Institute (IWII) Wound infection in clinical practice. Wounds International 2016)
4. What if the infection is under control but the wound still doesn’t heal?
It is extremely important to look at a patient holistically when we are considering why a wound is not healing. If they have diabetes is their blood sugar control optimised? Do they have an adequate diet and are eating the key food groups such as proteins? Are there any other underlying medical issues such as anaemia and low vitamin D? Has the patient got an adequate blood supply to the area where the wound is present? Is the patient being concordant with the treatment plan? Is the area where the wound is present being offloaded from any excess pressure. The wound must also be assessed as it is likely to be stuck in the “inflammatory” phase of healing.
“A large proportion of wounds are at risk of becoming stalled because of the presence of a biofilm.”
Biofilms are formed when microorganisms attach to the wound surface and then secrete a polysaccharide coating (EPS). Clinicians need to take into consideration that not all dressings have a biofilm indication. Podiatrists can disrupt biofilms by debriding but we also locally use Prontosan Solution at each dressing change to aid removal and reformation of the biofilm. If the patient is shared care between podiatry and nursing staff the Prontosan Debridement Pads can be used by the nurses to debride the wound and disrupt the biofilm. Prontosan Gel X can then be used as the primary dressing to prevent the formation of a biofilm and prevent infection.
This blog is an adaption of work submitted for an article original published by Practical Patient Care
Original Article
REFERENCE
1. Guest JF, Fuller GW, Vowden P. Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open 2020; 10:e045253