Total intravenous anesthesia (TIVA)
Total intravenous anaesthesia (TIVA) is a technique of general anaesthesia which uses a combination of agents given exclusively by the intravenous route without the use of inhalation agents (Gas Anaesthesia)1.
There is a solid rationale for the use of TIVA in some patient cases where the delivery of inhaled anesthetics is impossible or disadvantageous, or in scenarios where traditional anaesthetic delivery systems may be unavailable or impractical. In other cases, the use of TIVA could make the process more efficient and advantageous for the patient.
Compared generally to traditional volatile anaesthetic techniques, TIVA offers several potential advantages. These include reduced incidence of post-operative nausea and vomiting, reduced atmospheric pollution, more predictable and rapid recovery, greater haemodynamic stability, preservation of hypoxic pulmonary vasoconstriction, reduction in intracerebral pressure and reduced risk of organ toxicity.
In recent years, TIVA has become more popular, practical and possible due to two main reasons - firstly, the pharmacokinetic and pharmacodynamic properties of drugs such as Propofol and newer short-acting opioids, which make them suitable for intravenous administration. Secondly, new concepts in pharmacokinetic modeling coupled with advances in the technology of infusion pumps which allow the use of algorithms such as Target Controlled Infusion (TCI)2.
In comparison to traditional inhalation anaesthesia, the inherent benefits of TIVA via a Target Controlled Infusion (TCI) make it a more straightforward and user-friendly technique for the caregiver, while at the same time offering a faster and more comfortable patient recovery3.
TIVA is purely an anaesthetic technique, when used in cases where post-operative pain management will be required, multimodal pain management strategies could be applied such as conducting regional anaesthesia prior to the TIVA for post-operative use to improve patient recovery4.
Prescription
TIVA can be conducted either with a single drug or with a combination of drugs. The pharmacological profile (pharmacokinetics) of the drug help clarify it’s clinical implications and thus assist in drug selection. The most commonly utilised groups of drugs include hypnotics and short-acting opioids5. The discovery of Propofol in the 70s revolutionised the use of TIVA. It is currently the only intravenously active hypnotic agent suitable for the induction & maintenance of anaesthesia. Propofol-based TIVA techniques offer many advantages including rapid recovery of consciousness and psychomotor function, enhanced recovery speed, anti-emetic effect and a lower incidence of post-operative nausea and vomiting6. The Propofol can be coupled with opioids, muscle relaxants, NSAIDs etc. depending on the patient case or the type of procedure to be performed. When using TIVA via TCI, short-acting opioids such as Remifentanil are preferred. Recently, it was seen that TIVA via a TCI combining Remifentanil & Propofol effectively controlled intra-operative responses while allowing for rapid emergence from anesthesia in elective inpatient surgery7. Similar results have also been noted in outpatient surgeries.
Related Products – Prescription
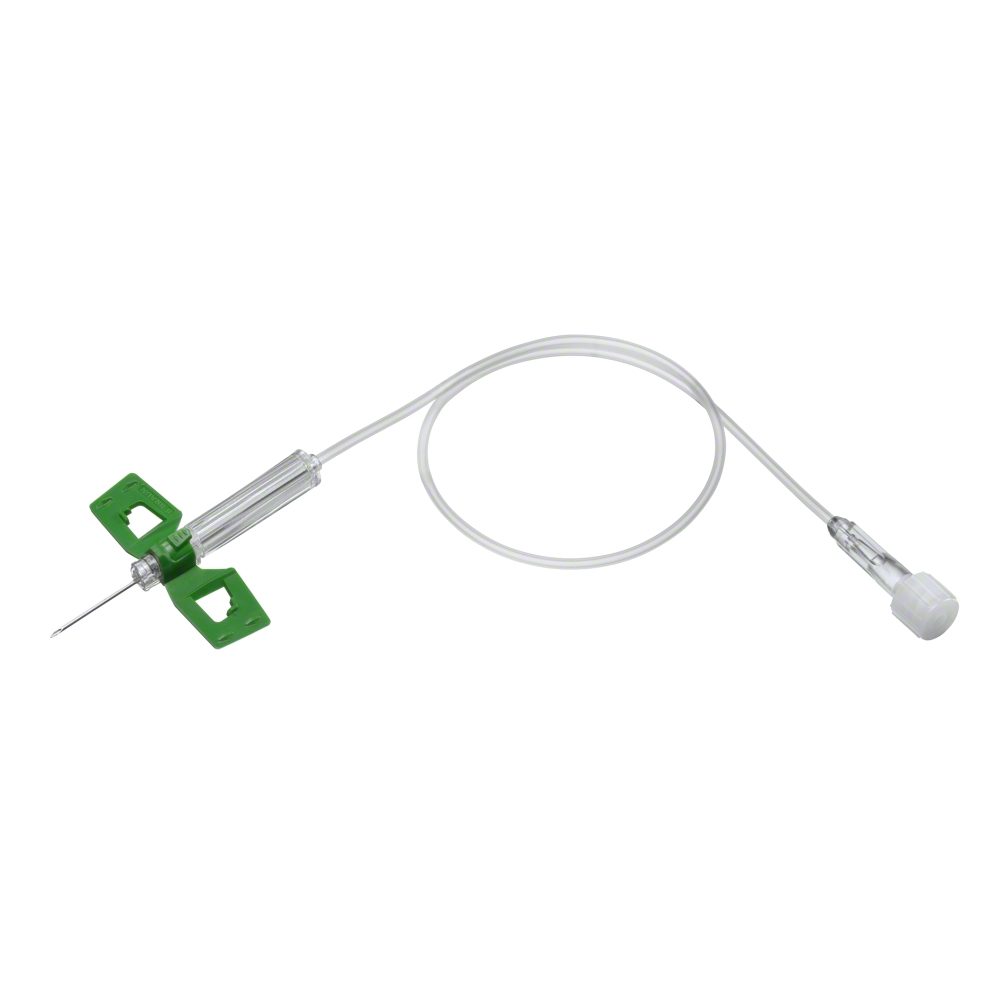
Patient Access
As TIVA is conducted exclusively via an intravenous infusion, the choice must be made from either a peripheral or a central venous access device. This selection is often guided either by the patient condition, or by the number and types of drugs being infused. For short term procedures, where extended venous access is not considered necessary, an Intravenous Catheter could be used. For patients where it is expected that post-procedure infusions would be required (for e. g. in critically ill patients), or in patients receiving a regimen of mutually-incompatible drugs, a multi-lumen central venous catheter is recommended. For neonatal or paediatric patients, a scalp vein set could also be used as an access device.
Preparation
The methodology of performing a TIVA via TCI depends highly on the choice or regimen of drugs selected which also consequently influences the drug preparation process. The selected drugs may or may not be available in ready-to-use glass/plastic vials, or glass/plastic ampoules. Ready-to-use drugs can be drawn up into syringes directly or through a filter. For drugs that need mixing, needle-free mixing devices and mixing bags could be used. In some cases, process-specific procedure kits could be made available which include all the necessary devices, drapes and dressings, based on the choice of method or drug combination. These procedure kits could support in making the entire process safer and more efficient.
Application
As with drug preparation and patient access, the drug application device is also indicated by the choice of method and choice of drugs used in the TIVA. For induction, or the injection of analgesic prior to the induction of anaesthesia, a syringe could be used. For the anaesthesia conducted via a TCI algorithm, a smart syringe pump could be used. The sophistication of syringe infusion pumps has developed rapidly in the recent past. Current pumps offer an inbuilt TCI algorithm functionality with common algorithms for the most widely used TIVA drugs. The pumps also have dedicated syringes and extension lines allowing more than one drug to be infused simultaneously. A 3-way stopcock could also be used in order to combine or split
Discharge Management
TIVA in itself does not support post-operative pain management, however if used in a multimodal pain management approach such as in combination with regional anaesthesia, continued analgesia can be provided. If no regional anaesthesia is conducted or if post-operative pain can be managed via the infusion of IV analgesics, the same smart pump can immediately be switched over to this therapy thus helping to improve patient satisfaction.
References
- ‘Total Intravenous Anesthesia using a target controlled infusion – A pocket reference’, College of Anesthesiologists, Academy of Medicine Malaysia (retrieved 07.10.15).
- Campbell, L., Engbers, F. H., & Kenny, G. N. (2001). Total intravenous anaesthesia. CPD ANAESTHESIA, 3(3), 109-119.
- Ozkose, Z., Ercan, B., Ünal, Y., Yardim, S., Kaymaz, M., Dogulu, F., & Pasaoglu, A. (2001). Inhalation versus total intravenous anesthesia for lumbar disc herniation: comparison of hemodynamic effects, recovery characteristics, and cost. Journal of neurosurgical anesthesiology, 13(4), 296-302.
- Aunac, S., Carlier, M., Singelyn, F., & De Kock, M. (2002). The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesthesia & Analgesia, 95(3), 746-750.
- Nora, Fernando Squeff. (2008). Total intravenous anesthesia as a target-controlled infusion: an evolutive analysis. Revista Brasileira de Anestesiologia, 58(2), 179-192. Retrieved October 07, 2015, from http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-70942008000200011&lng=en&tlng=en. 10.1590/S0034-70942008000200011.
- Absalom A & Struys M. An Overview of TCI & TIVA. Second Edition., 2011; Gent: Academia Press
- Hogue, C. W., Bowdle, T. A., O'Leary, C., Duncalf, D., Miguel, R., Pitts, M., ... & Batenhorst, R. (1996). A multicenter evaluation of total intravenous anesthesia with remifentanil and propofol for elective inpatient surgery. Anesthesia & Analgesia, 83(2), 279-285.