No content results match your keyword.
Content
You have successfully logged out.
Not registered yet?
RENU Managed Equipment Service
Healthcare is evolving, and the operating theatre is central to that shift. Whilst it is an essential hub for life-saving care, it is also a significant source of waste and overconsumption of valuable equipment. Every single-use instrument carries a hidden cost that is not just financial, but environmental. With surgical volumes rising and supply chains under strain, the NHS is well-placed to drive more sustainable practices. B. Braun’s RENU Managed Equipment Service has helped NHS hospitals avoid over 6,000 single-use instruments in a single year, saving more than £218,000 and 723 kg of waste1.
Despite being the first healthcare system globally to have Net Zero embedded into legislation, the NHS is responsible for around 4% of England's carbon footprint, with up to 66% of the emissions coming from the supply chain2. Operating rooms have a huge part to play in this, accounting for 20-30% of hospital waste, largely due to the widespread use of single-use items such as surgical steel instruments3. For an individual laparoscopic cholecystectomy, single-use instruments are estimated to account for 22.7 kg CO2e per case, highlighting the environmental burden. Financially, the impact is just as stark: devices like harmonic shears cost over £500 each, yet around 90% are discarded after a single use4. This reliance on disposables creates a cycle of unnecessary cost and carbon emissions – a challenge that sustainable alternatives can help break.
The Design for Life roadmap, created and published by the Department of Health & Social Care in 2025, emphasises the need for a circular economy in MedTech. Its goal: reduce waste and strengthen supply chains by prioritising reuse, remanufacture and recycling. By adopting systems that extend the life of surgical instruments and reduce waste, hospitals can lower emissions, cut costs, and build resilience into their supply chains5.
For clinicians, the environmental case for reusable instruments is compelling. A life cycle assessment, comparing stainless steel disposable scissors with reusable alternatives over 4,500 use cycles, found that disposables generate 99% more environmental impact6. This difference is driven by the repeated manufacturing, transport, and incineration of single-use products – all resource-heavy and releasing significant emissions. Reusable, by contrast, consolidate their footprint into one initial production phase, supported by sterilisation processes far less resource-intensive than manufacturing thousands of new instruments.
Avoided over
0
single-use instruments in a single year1
More than
£ 0K
in savings1
Saving
0kg
of waste1
The potential of reusable surgical instruments is dependent on proper maintenance and quality assurance to ensure patient safety and operational reliability. A review of 65 audits across 48 hospitals over two and a half years, checking 32,000 reusable instruments, found that 31% needed replacement, 33% needed repair, 18% had surface finish issues such as corrosion or water marks - and only 18% were acceptable and deemed fit for use7. Equipment that is decommissioned due to age, poor maintenance, damage or loss can put patient safety at risk by delaying operations or by forcing cancellation of procedures when instruments aren’t available 7.
To ensure a long life for reusable surgical instruments, whilst protecting the safety of both patients and healthcare staff, equipment must be inspected, repaired and maintained. This can be preventive or corrective, and both forms of maintenance are vital. Planned preventative maintenance involves servicing the instruments at regular intervals to extend their life and reduce failure rates. Corrective maintenance, sometimes referred to as ad hoc repair, is the process of repairing medical devices after a fault has been detected, restoring its functionality so it can be put back to use.
B. Braun’s RENU managed equipment service provides surgical staff access to high quality surgical equipment, including instruments, endoscopes, trocars and power systems. These services help reduce reliance on single-use instruments by providing access to reusable alternatives under a fixed-cost model. This approach not only supports more predictable budgeting, but enables long-term savings by avoiding the continuous repurchase of disposable items. RENU supports in streamlining surgical workflows by ensuring all necessary instruments are provided in a consolidated set, enabling storage in one central location on site.
Surgical teams can work with B. Braun to develop instrument sets tailored to clinical needs, with flexibility to add or adjust components as required. Sets are typically recalled at regular intervals for planned maintenance, where instruments are inspected, repaired, refurbished, or replaced if damaged beyond repair.
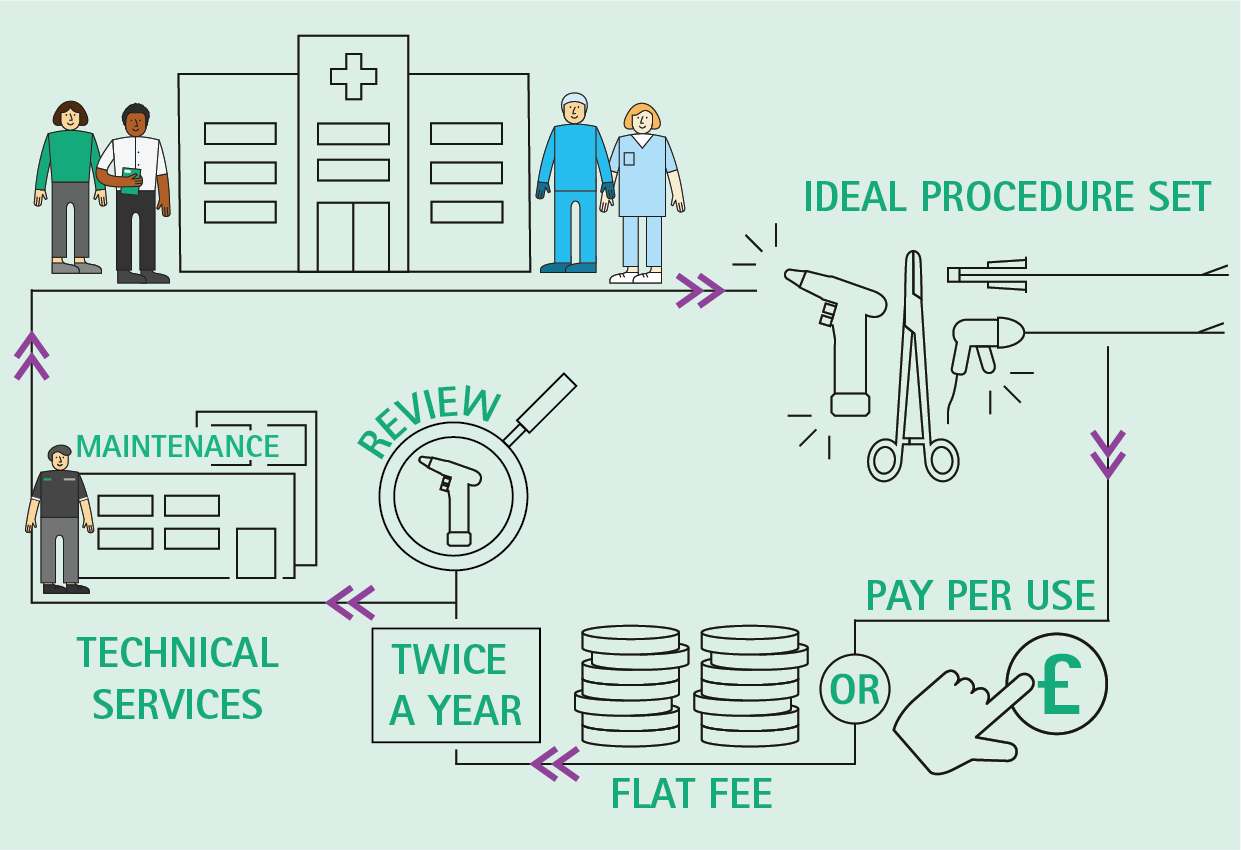
In the case of B. Braun’s RENU service, instruments aim to be returned to hospitals within five working days to minimise disruption or delays to surgical schedules. Data from the managed equipment service shows an instrument repair rate of up to 81%8, with an average replacement rate of 15%, compared with 34% for those repaired ad hoc9.
Post-COVID procurement issues, supply chain disruptions and daily uncertainty over instrument availability created significant operational pressures at Queen Elizabeth Hospital, Gateshead Health NHS Foundation Trust. To overcome these challenges, a multidisciplinary team of surgeons, operating department practitioners, and sterile services staff worked together to find a sustainable solution. The team carried out an initial 4-week trial in General Gynaecology of reusable laparoscopic equipment from the RENU service, including a bi-polar device. This was followed by a phased rollout designed to introduce change gradually, maintain training and engagement for both clinical and central sterile services department (CSSD) staff and prioritise patient safety during the transition:
Phase 1: Gynaecological laparoscopic tray implementation
Phase 2: General laparoscopic tray implementation/adjustments to Phase 1 trays to accommodate Gynae-Oncology
Phase 3: Partial implementation of reusable laparoscopic trocars
Phase 4: Complete roll out of all instruments with full uptake of reusable trocars
Each rollout phase delivered measurable results - avoiding the use of a significant number of disposable instruments (Figure 1) and generating substantial cost savings (Table 1).
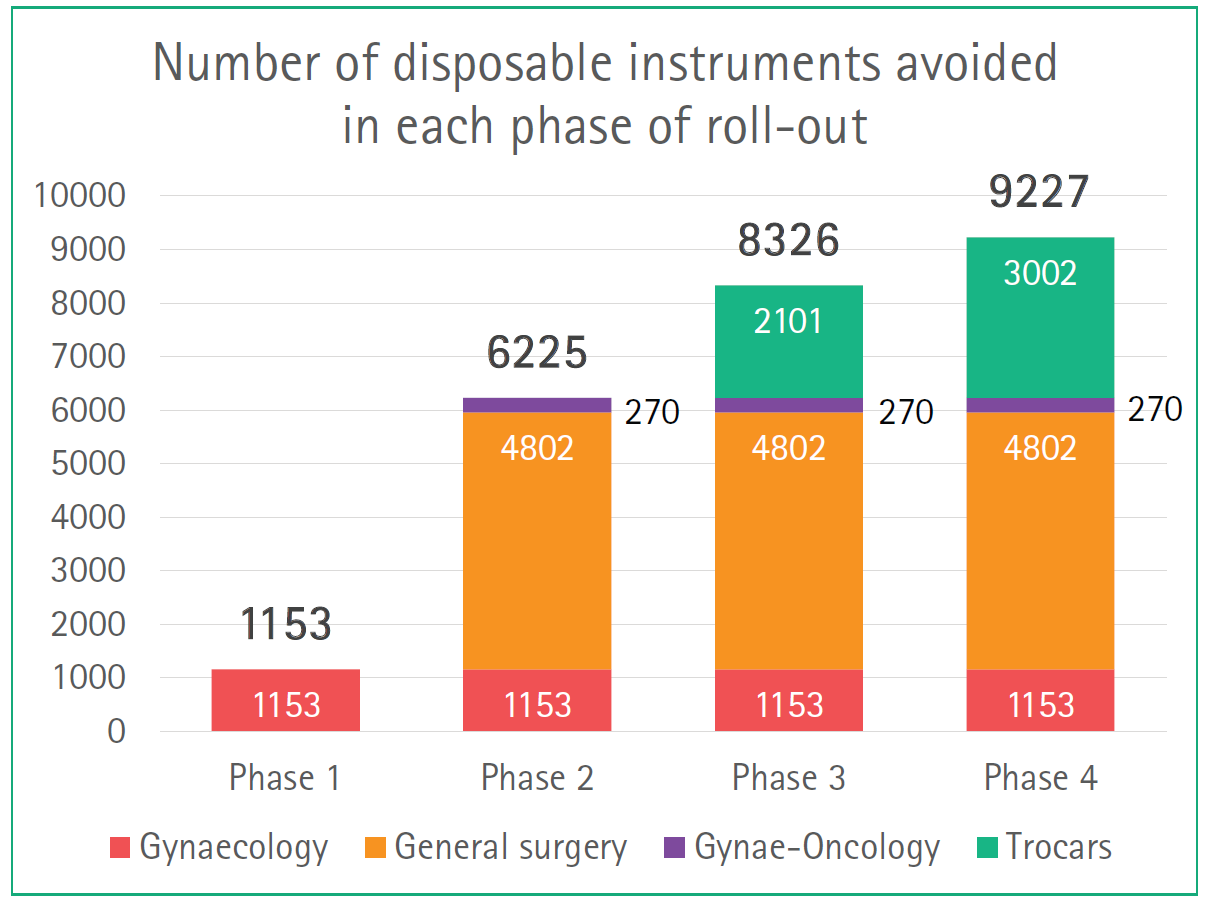 Source: Knightley et al
Source: Knightley et al
Phase | Annual savings |
Phase 1: Gynaecological laparoscopic tray
| £53,372 |
Phase 2: General laparoscopic tray Adjustments to Phase 1 trays to accommodate Gynae-Oncology
| £144,713 (in General Surgery) A further £20,034 per year (in addition to Phase 1 savings) Cumulative saving: £218,119 |
Phase 3: Partial implementation of reusable laparoscopic trocars
| Predicted annual saving of £100,229 (in addition to Phase 1 and 2 savings) Cumulative saving: £318,348 |
Phase 4: Complete roll out of all instruments with full uptake of reusable trocars
| Predicted annual savings of £163,466 (in addition to Phase 1 and 2 savings) Cumulative saving: £381,585 |
The annual spending on disposable instruments in Phase 1 and 2 was previously £380,195, which fell to £162,077 in the first year of the RENU service contract, a saving of £218,119 in the 12 months of Phase 2 (Figure 2). The team estimates total annual savings of £381,585 by the end of Phase 4.
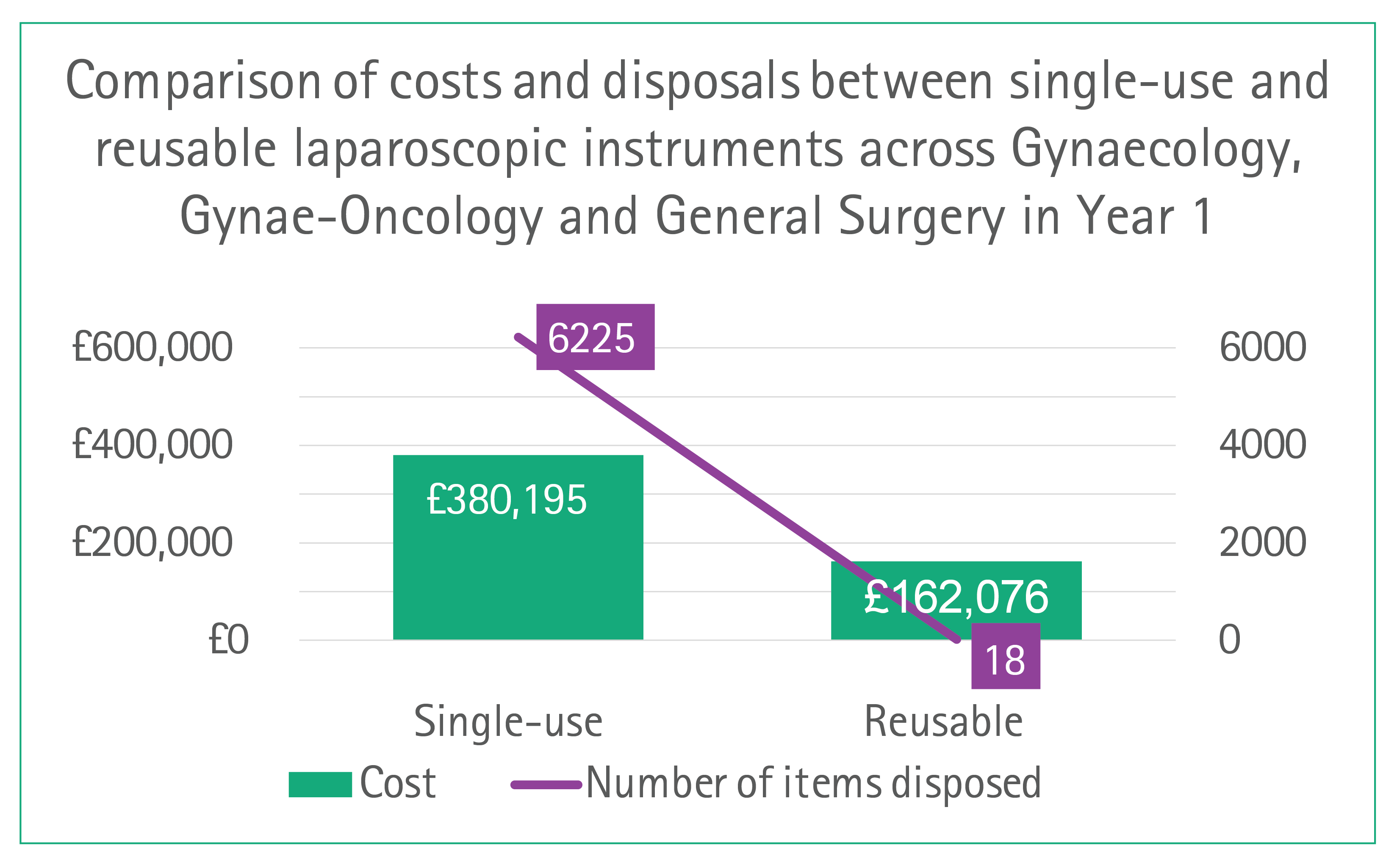 Source: Knightley et al
Source: Knightley et al
The savings were not just financial. At the Queen Elizabeth Hospital, the single-use items were stored separately, requiring around an hour of equipment gathering by two members of the logistics team in preparation for surgery. With the introduction of the RENU service, all instruments were consolidated into a single bespoke tray, reducing preparation time to just 10 minutes for one staff member, freeing up valuable time for other tasks1.
Adopting reusable laparoscopic instruments is a pivotal strategy for advancing environmental sustainability in surgical practice. This approach reduces reliance on single-use plastics, minimises waste generation, and supports healthcare systems in meeting carbon reduction targets. Over a year, the Queen Elizabeth Hospital performs around 1,152 laparoscopic procedures across General Surgery, General Gynaecology and Gynae-Oncology, with each procedure using between three and seven laparoscopic instruments. By switching from single-use to reusable instruments, the hospital has saved 6,225 instruments from disposal in a year (Figure 2), with a combined weight of 723.2 kg. By Phase 4, an additional 3,000 single-use plastic trocars, weighing around 390 kg, were also avoided.
The service would not work without buy-in from the surgical staff. In a survey of 11 general surgeons and gynaecological surgeons, most or all rated the devices as excellent, very good or good based on weight/balance, ergonomics, insertion, fixation, transition and performance1. Crucially, the feedback confirmed that switching to reusable instruments did not compromise surgical quality - reinforcing that sustainability and high clinical standards can go together.
The shift to a circular economy in healthcare is no longer optional - it is essential. Transitioning to reusable surgical instruments delivers a dual benefit: it dramatically reduces environmental impact, while unlocking significant financial savings for hospitals. B. Braun’s managed equipment service makes this transition practical and scalable by ensuring instruments are maintained to the highest standards, extending their lifespan and guaranteeing clinical quality. This service model equips surgical teams with reliable, fit-for-the-future tools that improve patient experience and free resources for frontline care. By using B. Braun RENU, hospitals can move beyond incremental change and embed sustainability at the heart of surgical practice - protecting both people and the planet, while safeguarding the financial health of our NHS.
1. Knightley, L., B. Dent, and I. Cameron, Financial and environmental impact of the introduction of reusable laparoscopic instruments, in BADS Annual Conference 2025. 2025: University Place, Manchester.
2. Reducing the environmental impact of equipment, medicines and resources. Last accessed: 16 October 2025. Available from: https://www.england.nhs.uk/ahp/greener-ahphub/specific-areas-for-consideration/reducing-the-environmental-impact-of-equipment-medicines-and-resources.
3. Bolten, A., et al., The carbon footprint of the operating room related to infection prevention measures: a scoping review. J Hosp Infect, 2022. 128: p. 64-73.
4. Streeting, W., Major crackdown on NHS waste. Department of Health and Social Care 16 October 2024. Available from: https://www.gov.uk/government/news/major-crackdown-on-nhs-waste.
5. Policy paper: Design for Life roadmap. Department of Health & Social Care. 31 January 2025. Available from: https://www.gov.uk/government/publications/design-for-life-roadmap/design-for-life-roadmap--4.
6. Ibbotson, S., et al., Eco-efficiency of disposable and reusable surgical instruments—a scissors case. Sustainable Development, 2013. 18: p. 1137–1148.
7. Quality, Safety and Value: The role of surgical instruments. ABHI. June 2020. Available from: abhi-the-role-of-surgical-instruments.pdf
8. B. Braun Real World Evidence Team, Technical Services Instrument Repair Audit. 2024.
9. Data on file. B. Braun.